1801006185 long case : 45 yr old male patient with heart failure .
1801006185 long case : 45 year old male patient with heart failure .
A 45 old male patient auto driver by occupation came to the OPD with cheif complaints of swelling in the both legs & shortness of breath since 5 days.
History of present illness:
Patient was apparently asymptomatic 5 days back then he developed increased swelling in both lower limbs which is pitting type of edema .insidious in onset gradual in progression. Swelling is up to the ankles . It is not seen above the ankles .
patient also complains of shortness of breath which is insidious onset gradually progressive . It progressed from grade 2 to grade-4.Patient also complains of breathlessness in lying down position. Aggravated on activity and relived on rest .
History of paroxysmal nocturnal Dyspnea is present 3 hours after patient sleeps and it is relieved when patient arises.
Patient also complains of fatigue on activity.
No complaints of facial puffiness .
No H/o chest pain , palpitations, syncope attack .
No complaints of confusion , altered mental status , lack of concentration , memory impairment .
No complaints of abdominal pain .
No H/O cough , sputum , hemoptysis, chest pain.
No H/O burning micturation , increased frequency of urine , decreased urine output .
Past history:
Similar complaints are seen 7 months back for which he is undergoing hemodialysis (twice aweek).
Patient is known case of diabetic since 6 years .Patient is also hypertensive since 5 years . No history of tuberculosis, asthma , epilepsy .
Treatment history:
patient is taking insulin injections for the diabetes and for hypertension he is taking Tab clinidipine,Tab furosemide, Tab metaprolol .
Personal history:
Appetite is normal, diet is mixed , bowel and bladder are regular, sleep is adequate, and no addictions & no allergies.
Family history:
no similar complaints in the family.
General examination:
Patient is conscious,coherent & cooperative. Moderately built and well nourished , well oriented with time , place and person.
Pallor is present
No icterus , cyanosis , clubbing , lymphadenopathy.
Pedal edema is present.
Vitals:
Temperature:98.6°f
Pulse rate:82b/m
Blood pressure:130/80mmhg.
Respiratory rate:18 cycles/min.
Systemic examination:
CVS Examination:
Inspection:
JVP is raised.
Chest wall is bilaterally symmetrical. No precordial bulge, no engorged veins over the chest wall , no engorged neck veins , tracheal position is central . No scars and sinuses .
Palpation :
Apex beat is present at the 8th intetcostal space 1cm lateral to the mid clavicular line .
No pulsations, No parastetnal heave , No precordial or carotid thrill , No dilated veins .
Percussion : normal
Auscultation: s1and s2 are heard and no murmurs.
Respiratory system examination:
Inspection:
Upper respiratory tract : oral cavity , nose , pharynx are normal.
Lower respiratory tract :
Chest is bilaterally symmetrical , No chest deformities, No spinal deformities, Movements of the chest are symmetrical.
Palpation :
Apex beat at the level of 8th intercostal space 1cm lateral to the midclavicular line .
Trachea is central in position, Chest expansion is normal , expansion of chest is bilaterally symmetrical. No tactile Fremitus and No friction fremitus. Vocal fremitus is also normal.
Percussion : resonant.
Auscultation:
Bilateral crepitations present in all areas .
Vocal resonance is normal , No wheezing , No stridor , No pleural and pericordial rub .
Per abdomen examination:
Inspection:
Abdominal distension is present . Fullness of flanks is seen .
Umbilicus is inverted , all quadrants move equally with the respiration, No visible pulsations , No scars , sinuses , striae , stretched skin, No hernial orifices , No veins on the abdominal wall .
Palpation :
No rise of temperature and No tenderness over the abdomen .
No enlargement of organs .
Percussion : shifting dullness is present , No fluid thrill , No increase in the liver span .
Auscultation:
Bowel sounds are heard .
CNS examination :
Higher mental functions are normal .
Cranial nerves examination is normal .
Motor system :
1. Bulk : both right and left upper and lower limbs are normal .
2.Tone : tone of both upper and lower limbs are normal .
3. Power : power of neck muscles , upper limbs , lower limbs, trunk muscles are good .
4. Reflexes : superficial reflexes are normal .
Deep tendon reflexes : Biceps jerk , triceps jerk , ankle jerk , knee jerk are present .
Normal gait and No involuntary movements.
Sensory system : crude touch , pain , temperature, fine touch , vibration , position sense are normal .
Cerebellar signs : Nystagmus , Dysarthria , Hypotonia are not present .
No signs of meningeal irritation.
Provisional diagnosis : Heart failure with pulmonary edema .
INVESTIGATIONS:
Hemogram:
Hb: 9.5gm/dl ( 13-17)
Mcv : 80.8fl (83-101)
Mch: 26.5pg (27-32)
Rbc count : 3.59millions/cumm (4.5-5.5)
RFT:
Urea : 56mg/dl (12-42)
Creatinine : 6.8mg/dl (0.9-1.3)
LFT:
Alkaline phosphate : 210IU/L (53-128)
Albumin :3.23gm/dl (3.5-5.2)
Serum iron: 60micrograms/dl .
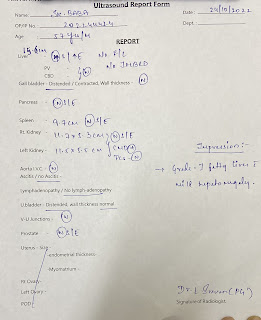
2D echo:
Chest x-ray :
CKD .
Anemia of chronic disease.
Treatment:
Bed rest .
Fluid restriction <1.5 lit/day
Salt restriction < 2gm/day
Inj.Lasix 40mg IV/BD.
Inj.20FER 4mg IV/OD.
Inj.pan 40mg IV/OD.
Moniter vitals.







Comments
Post a Comment